Diabetic Retinopathy Care in Chattanooga, Knoxville, and the Tri-Cities Region
Diabetic retinopathy is a complication of Diabetes Mellitus, in which elevated blood glucose levels damage the retina’s tiny blood vessels. Without treatment, this condition can lead to vision loss and even permanent blindness. Diabetic retinopathy is the most common cause of vision loss in adults with Diabetes Mellitus and may develop with either type 1 or type 2 diabetes. At Southeastern Retina Associates, we provide advanced surgical and nonsurgical treatment options to help reduce additional damage and potentially restore retinal function.
What is Diabetic Retinopathy?
Diabetes Mellitus is a chronic condition that negatively impacts your body’s ability to control blood glucose levels. For the retina, this chronic high blood sugar can damage the walls of its blood vessels, weakening them. This can cause microaneurysms (i.e., small red bulges) to form in the vascular tissue, as well as incompetent walls of the blood vessels. Microaneurysms are prone to leaking blood and blood components into the retina which can cause excessive edema, or swelling, in the retina. When this occurs in the macula, the central portion of the retina, it may affect your central vision or reading vision.
Due to this damage, your retina and other parts of your eye may be deprived of crucial blood and nourishment. Over time, abnormal new blood vessels start to grow in an attempt to replenish the lost blood and nutrients through a process called neovascularization. However, these new blood vessels are extremely delicate and weak; instead of supporting the retinal vascular system, they bleed and leak into the retina and vitreous cavity. The vitreous cavity is usually filled with a clear fluid that allows light to pass through to your retina.
Types of Diabetic Retinopathy
With diabetic retinopathy, there are two main types.
Nonproliferative diabetic retinopathy (NPDR) — The earlier form of diabetic retinopathy. In its earliest stages, many patients with NPDR may not know they’re afflicted as there may be no symptoms.
Proliferative diabetic retinopathy (PDR) — The more advanced form of diabetic retinopathy, in which neovascularization occurs. Abnormal vessels may develop underneath the retina and within the vitreous gel that fills the eye.
Symptoms of Diabetic Retinopathy
As diabetic retinopathy progresses, blockages in retinal blood vessels may result in such symptoms as:
- Blurred vision
- Decreased clarity
- Fluctuating vision quality
A related condition, diabetic macular edema (DME), may also develop with NPDR. Should diabetic retinopathy progress to the more advanced PDR type, you may experience symptoms such as eye floaters, hazy vision, and issues with night vision and lighting.
If untreated, diabetic retinopathy can lead to several complications, including:
- Neovascular glaucoma – Blood vessel growth on the iris (i.e., the eye’s colored part) and in the eyes’ drainage channels
- Retinal detachment – Because these new blood vessels are fragile, they easily bleed, forming scar tissue, which can pull the retina partially or completely out of position
- Vitreous hemorrhage – Heavy bleeding can develop within the vitreous, causing floaters or blocking vision, although this may be temporary
- Permanent blindness
- The loss of an eye
As NPDR can advance to the PDR type, it’s essential to regularly monitor your retinal health and undergo a comprehensive diabetic eye exam at least once a year.
Diabetic Retinopathy Risk Factors
While anyone with type 1 or type 2 diabetes may develop diabetic retinopathy, your likelihood may increase if you also have the following risk factors:
- Having Diabetes Mellitus for a long time
- Not having proper control over your blood sugar levels
- High blood pressure
- High cholesterol
- Tobacco use
- Obesity
Diabetic Retinopathy FAQ
It’s estimated that about 9.6 million people in the United States have diabetic retinopathy, which accounts for about 26.34% of patients with Diabetes Mellitus. However, diabetic retinopathy may be even more common; since patients with early onset NPDR typically don’t experience symptoms, there’s no telling how many people have the condition without realizing it. This is one of the reasons why getting regular diabetic eye exams is so crucial.
With NPDR, you may be at risk for a condition called diabetic macular edema (DME), which develops when fluid or blood accumulates in the macula, and may cause swelling and problems with central vision. If untreated, DME may lead to blindness and permanent retinal nerve cell damage.
Anyone with any Diabetes Mellitus type is advised to have a comprehensive eye exam from a diabetic eye specialist at least once a year. However, your specific Diabetes Mellitus type may determine additional exam frequency, particularly for follow-ups. Those with type 1 diabetes are advised to schedule an eye exam with an eye doctor within five years of their diagnosis. If you have type 2 diabetes, you should schedule an exam at the time of diagnosis. These visits enable early detection and treatment, hopefully, before vision loss has occurred, and are determined by your doctor.
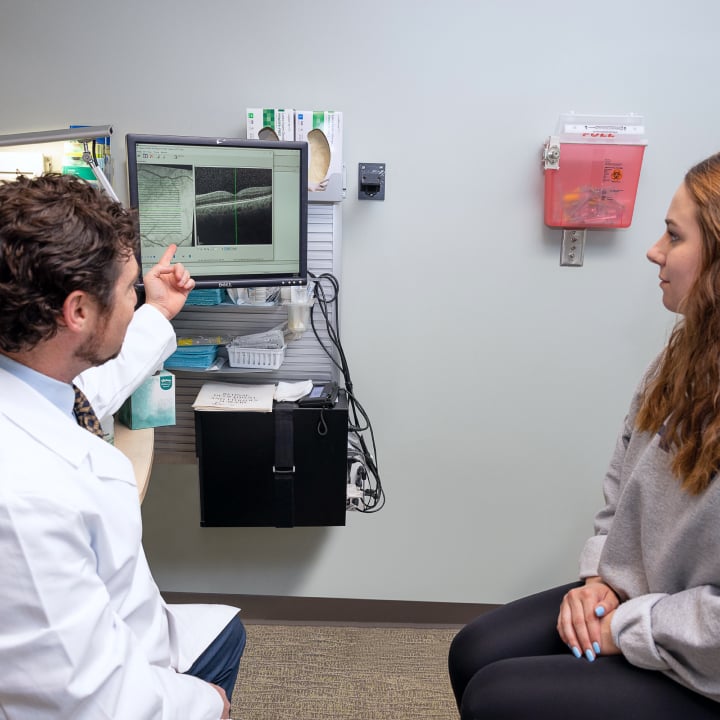
Expert Care for Diabetic Retinopathy at Southeastern Retina Associates
Anyone with Diabetes Mellitus may be at risk for the development of diabetic retinopathy. At Southeastern Retina Associates, our diabetic eye specialists have the necessary experience, skills, and technology to diagnose and treat patients with all levels of diabetic retinopathy. Contact us today to request a consultation for diabetic retinopathy.


